On November 1, 2019, the Centers for Medicare & Medicaid Services (CMS) released CY 2020 Revisions to Payment Policies under the Physician Fee Schedule and Other Changes to Part B Payment Policies [CMS-1715-F and IFC], which includes changes related to Medicare physician payment and the Quality Payment Program (QPP) effective for services on January 1, 2020. The final regulations will be published in the Federal Register on November 15, 2019. Comments for this rule will be accepted only on the interim rule’s “Coding and Payment for Evaluation and Management, Observation and Provision of Self-Administered Esketamine” section and are due on December 31, 2019.
With little change in the physician conversion factor for CY 2020, Medicare physician payments are expected to remain relatively flat. Although, with changes to work, practice expense and malpractice relative value units (RVUs), the aggregate impact of changes from the 2020 physician final fee schedule (PFS) will vary by specialty and service mix.
In one of the final rule’s most significant changes, CMS adopted coding changes and payment increases for evaluation management (E/M) codes effective in 2021. Also in 2021, CMS will begin transitioning clinicians from its current Merit-Based Incentive Payment System (MIPS) program to the newly established MIPS Value Pathways (MVP) framework. In characterizing the rule, the administration highlighted its efforts to “secure and improve Medicare and establish a patient-driven healthcare system that focuses on improving health outcomes.” CMS noted that the rule is expected to save clinicians 2.3 million hours per year through reduced administrative burden.
Key Takeaways
1. The 2020 physician conversion factor remains flat at $36.0896.
2. CMS increases payment for evaluation and management services in CY 2021.
3. CMS increases payment for transitional care management services.
4. CMS expands opioid use treatment services through multiple policies.
5. MIPS score to avoid negative update increases for CY 2020 (2022 payment year).
Medicare physician payment is based on the application of the dollar conversion factor to work, PE and malpractice RVUs, which are then geographically adjusted.
Key Takeaway: 2020 Physician Conversion Factor Remains Flat at $36.0896.
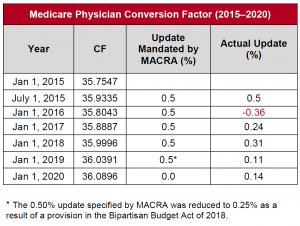
This figure represents an increase of just five cents from the 2019 physician conversion factor of $36.0391. The proposed anesthesia conversion factor is $22.2016, in comparison to the 2019 conversion factor of $22.2730, representing a reduction of seven cents. Because the annual update to the physician conversion factor authorized by the Medicare Access and CHIP Reauthorization Act (MACRA) expired in 2019, there was no statutorily required update of this conversion factor. However, CMS applied an RVU budget neutrality adjustment (0.14%) to both conversion factors, and applied a PE and malpractice adjustment (-0.46%) to the anesthesia conversion factor.
MACRA replaced the Sustainable Growth Rate Formula and established the framework for a physician quality reporting program. MACRA was also intended to create year-to-year stability in Medicare payment. Since the establishment of MACRA, in all but one year various adjustments scaled back the 0.5% MACRA updates scheduled for CYs 2015–2019, yet the conversion factor has remained relatively stable, hovering around $36.
PE RVUs capture the cost of supplies, equipment and clinical personnel wages used to furnish a specific service. In addition to work RVU changes to new or revised CPT codes, in this final rule CMS also implemented a series of standard technical proposals involving PE, including the implementation of the second year of the market-based supply and equipment pricing update, and standard rate setting refinements to update premium data involving malpractice expense and geographic practice cost indices.
The overall impact of these changes varies by specialty. CMS estimates that the impact ranges from a negative 4% for ophthalmology to a positive 4% for clinical social workers.
Key Takeaway: CMS will adopt CPT coding changes and RUC recommended values for office/outpatient visit E/M codes for CY 2021. Assuming no further changes next year, this will increase RVUs for most office/outpatient E/M services. Payment rates for other services likely will be reduced in CY 2021. Increase in E/M RVUs do not extend to global surgeries.
In the CY 2020 Final Rule, CMS has finalized its proposal to adopt E/M coding recommendations from the CPT Editorial Panel for CY 2021.
CMS also finalized RUC-recommended work RVU values for the office/outpatient E/M visit codes for CY 2021 and the new add-on CPT code for prolonged service time. The RUC-recommended values yield higher work RVUs for most office/outpatient E/M services.
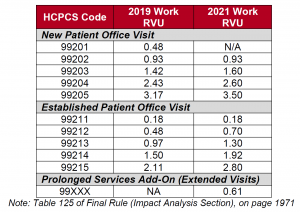
The impact of higher work RVUs on payment will not be known until the CY 2021 rulemaking schedule. Changes under the Medicare PFS are required to be budget neutral. To offset increased spending from the finalized E/M changes, CMS will need to make across-the-board reductions, which will likely be implemented through a reduction in the physician conversion factor. Reductions to the physician conversion factor will work to reduce payment for all services reimbursed under the PFS compared to rates without the budget neutrality adjustment.
The impact on specialties or individual practices will be driven by the mix of E/M services they bill. Specialties and practices that bill higher level established patient visits will see the greatest increases, as those codes were revalued higher relative to the rest of the office/outpatient E/M code set. Specialties and practices that do not generally bill office/outpatient E/M visits may experience greater decreases. While CMS published a specialty-specific impact table for CY 2021 (Table 120), the agency did not update estimates from the proposed rule because there are unknowns regarding other changes that will occur in CY 2021.
In the final rule, CMS acknowledged the “redistributive impact” of the finalized E/M changes as well as commenter concerns but indicated that it is premature to discuss strategies for mitigating the impact of these changes. CMS intends to further consider these concerns and address them in future rulemaking.
Under RUC methods, RVUs for surgeries with 10- and 90-day surgical global periods include RVUs for the number and level of E/M visits considered to be typically performed. However, CMS rejected the RUC recommendation to increase the RVUs of surgical services with 10- and 90-day global periods to reflect the changes made to RVUs for office/outpatient E/M visits.
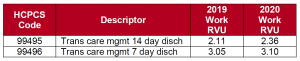
Key Takeaway: CMS increased payment for transitional care management (TCM) services and removed restrictions that had prohibited providers from billing care management codes with TCM services.
TCM services are provided to beneficiaries after an inpatient stay or certain outpatient stays. In recent years, CMS has worked to expand the codes that describe these services and improve their payments. For CY 2020, in response to an analysis that indicated low utilization of TCM services relative to the number of beneficiaries with eligible discharges, CMS finalized a proposal to increase payment for TCM services. To encourage utilization of these services, CMS will allow concurrent billing of the 14 codes currently restricted from being billed with TCM. These 14 codes are listed in Table 20 of the final rule.
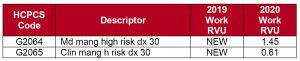
CMS finalized two new codes for 2020 for principal care management services that will pay clinicians for providing care management services to patients with a single serious and high-risk condition. The establishment of these codes recognizes that clinicians across specialties manage these type of patients.
CMS created a new code for additional time spent beyond the initial 20 minutes allowed in the current coding for chronic care management (CCM) services (G2058, Ccm add 20min, 0.54 work RVUs) and established a policy to allow for a single consent per year for communication-technology-based services rather than requiring the provider to obtain consent with each interaction. A care plan is required for billing CCM services. As part of its efforts towards burden reduction, CMS also finalized a simplified definition of a “typical care plan.”
Key Takeaway: CMS expanded opioid use treatment services, including via bundled payments, additions to the telehealth services list and coverage for medication assisted treatment (MAT).
US government agencies and communities across the United States have implemented strategies to address the opioid epidemic. In 2017, the US Department of Health and Human Services launched a five-point strategy that included better access to treatment. CMS finalized several proposals in the CY 2020 PFS that seek to expand access to opioid treatment services, including:
CMS will consider coding and payment amounts that recognize different levels of patient need and different types of practice arrangements for future rulemaking, including use of MAT in the emergency department setting.
Key Takeaway: Scope of practice for non-physician healthcare providers expanded as CMS relaxes supervision requirements.
Physician Assistants (PAs)
In CY 2018, CMS received comments providing examples of state law changes to PA supervision requirements. In response to comments and evaluation of current state law, CMS changed the physician supervision requirements for PAs.
PAs can now practice in accordance with state law. States may determine what level of supervision a PA requires when practicing in that state. If there are no such requirements established within a state, a PA must provide documentation, upon request, evidencing how the PA works with physicians.
Certified Registered Nurse Anesthetists (CRNAs)
Conditions for coverage for the ambulatory surgical center (ASC) environment require performance of a pre- and post-procedure assessment and a pre-discharge evaluation. The final rule expands the scope of professionals who may perform pre-surgery anesthesia risk assessment to include CRNAs. Previously, such a risk assessment was to be conducted by a physician. A physician must still perform the pre-surgery risk assessment for the procedure itself. CMS believes this expansion will decrease administrative burden, improve continuity of care and lower costs, while maintaining quality of care in the ASC setting.
Under the QPP, eligible clinicians elect either to be subject to payment adjustments based upon performance under MIPS or to participate in the Advanced APM track. Eligible clinicians choosing the MIPS pathway will have payments increased, maintained or decreased based on relative performance in four categories: Quality, Cost, Promoting Interoperability (meaningful use) and Improvement Activities. Eligible clinicians choosing the APM pathway will automatically receive a bonus payment once they meet the qualifications for that track.
Key Takeaway: MIPS score needed to avoid negative update increased for CY 2020, and CMS will transition to MVP framework beginning in CY 2021.
For the MIPS 2020 performance year (2022 payment year), CMS increased the performance threshold (i.e., the minimum MIPS score necessary to avoid a negative payment adjustment) to 45 points (from 30 points). CMS also finalized a performance threshold of 60 points for the 2021 performance year (2023 payment year).
CMS will begin to transition MIPS to the MVP framework beginning in CY 2021, in response to feedback from participating clinicians, a recommendation from the Medicare Payment Advisory Commission and the agency’s own analysis of the overall complexity of the program. Under the MVP, the clinician quality program will move away from reporting on activities and measures from the four performance categories (Quality, Cost, Improvement Activities and Promoting Interoperability) to a unified set of measures and activities centered around a specific condition or specialty.
CMS believes that because of its attempt to provide flexibility to clinicians in the initial years of the program, MIPS is now enormously complex and does not provide robust clinician performance information. Inherent in the concept of the MVP framework is a reduction in the number of MIPS quality measures, which is consistent with the agency’s Meaningful Measures initiative. Launched in 2017, that initiative has reduced the number of measures in a variety of Medicare and Medicaid quality programs.
Key Takeaway: Advanced APM policy continues to develop as stakeholders await announcement of additional models.
In the final rule, CMS commented that participation in Advanced APMs increased from 2017 to 2018. The number of qualifying APM participants almost doubled over that time, from 99,076 to 183,306. The final rule makes several technical changes to the QPP Advanced APM track, including adding a category of Aligned Other Payer Medical Home Models and modifying the definitions of marginal risk and expected expenditures for Other Payer Advanced APMs. The main area of activity with respect to Advanced APMs is expected to occur outside of this rulemaking with the release of additional payment models, including the Direct Contracting application, anticipated in the near future.
For more information, contact Sheila Madhani.