McDermott+ is pleased to bring you Regs & Eggs, a weekly Regulatory Affairs blog by Jeffrey Davis. Click here to subscribe to future blog posts.
March 27, 2025 – It’s March, which means one thing for sports fans: the madness of the NCAA men’s and women’s basketball tournaments. However, to folks in the regulatory world, it also means something else too: the Centers for Medicare & Medicaid Services’ (CMS’s) release of the Medicare 2026 proposed payment regs, the first fee-for-service rulemakings of the new Trump administration, is right around the corner. All in all, as the madness of the NCAA tournaments ends, the madness of reg season begins.
One of the most significant fiscal year (FY) Medicare payment regs is the Inpatient Prospective Payment System (IPPS) reg, which updates inpatient payment rates and establishes other policies for hospitals. To help provide a preview of the FY 2026 IPPS proposed reg, I’m bringing in my colleague Leigh Feldman. While Leigh is not as big a college basketball fan as I am (those who know me know that I’m pretty passionate), she, like me, appreciates the madness of reg season. Like the NCAA tournaments, it’s impossible to predict what will happen – but we’ll at least try to give you an overview of what to expect.
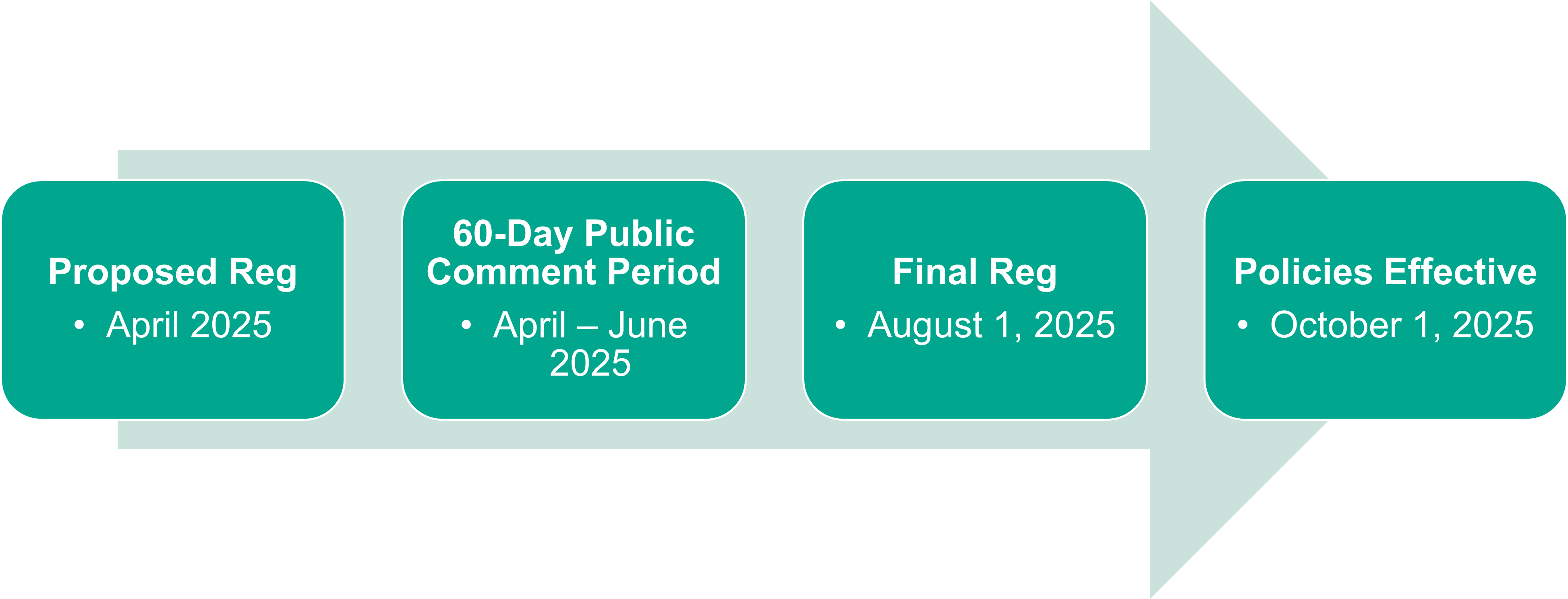
We expect CMS to release the FY 2026 IPPS proposed reg in early April 2025. The reg is currently being reviewed by the Office of Management and Budget, the final step in the regulatory review process. Once the proposed reg is released, there will be a 60-day public comment period, followed by release of the final reg on or around August 1, 2025. The reg’s policies will go into effect on October 1, 2025, the start of FY 2026.
Based on what this significant reg typically includes and the policies the first Trump administration supported, here are the major policies (the big three-point splashes, so to speak) that we are watching out for:
As discussed in last week’s Regs & Eggs blog post, this model likely will go forward – but it is definitely possible that CMS will propose changes to the model in this reg. Changes could include the elimination of certain model policies, payment adjustments, and requirements, as well as the addition of new ones. We expect that the Trump administration will try to put its own stamp on the TEAM model in alignment with some of the CMS Innovation Center’s new objectives that we discussed last week, including maximizing the potential for taxpayer savings.
As part of its Rethinking Rural Health initiative, the first Trump administration invited recommendations for changes to the Medicare wage index system in the FY 2019 IPPS proposed reg. Many responses to this solicitation reflected a concern that the wage index system perpetuates and exacerbates the disparities between high wage index hospitals, which tend to be urban, and low wage index hospitals, which tend to be rural.
CMS therefore adopted, in the FY 2020 IPPS reg, a “low wage index policy,” which increased the wage index for hospitals with a wage index value below the 25th percentile. An affected hospital had its wage index value increased by half the difference between the otherwise applicable wage index value for that hospital and the 25th percentile wage index value across all hospitals. CMS achieved budget neutrality for this change by adjusting payments across all IPPS hospitals. The agency indicated that this policy would be effective for at least four years.
However, the US Court of Appeals for the DC Circuit vacated the policy in Bridgeport Hosp. v. Becerra, holding that CMS lacked the authority it asserted to implement the low wage index policy. CMS issued an interim final reg in 2024 to recalculate the IPPS hospital wage index to remove the low wage index policy for FY 2025. The ball is in CMS’s court to come up with a new approach to address hospital wage index disparities going forward.
Failure to comply with a CoP results in loss of participation in the Medicare program, which makes CoPs one of the largest “sticks” that CMS has at its disposal.
The current administration hinted at its potential use of the CoP “stick” to advance its priorities with respect to gender-affirming care. Earlier in March, the Center for Clinical Standards and Quality (CCSQ), which serves as the focal point for all quality, clinical, and medical science issues and policies for CMS, released a Quality & Safety Special Alert Memo for hospitals, stating that CMS “may begin taking steps in the future to align policy, including CMS-regulated provider requirements and agreements, with the highest-quality medical evidence in the treatment of the nation’s children in order to protect children from harmful, often irreversible mutilation, including sterilization practices” (emphasis added). The memo was a first step toward the agency implementing section five of President Trump’s executive order (EO) “Protecting Children from Chemical and Surgical Mutilation,” which directs the US Department of Health and Human Services to take actions to “end the chemical and surgical mutilation of children, including regulatory and sub-regulatory actions,” including “Medicare or Medicaid conditions of participation or conditions for coverage, clinical-abuse or inappropriate-use assessments relevant to State Medicaid programs, and quality, safety, and oversight memoranda” (emphasis added).
If CMS addresses hospital CoPs around gender-affirming care in this year’s IPPS rule, it could also take the opportunity to revisit the new obstetric care and emergency readiness CoPs that the Biden administration finalized. Those CoPs require hospitals to put in place new emergency services readiness and transfer protocols; new rules for the organization, staffing, and delivery of services in obstetrical units; new obstetrical staff training; and updated quality assurance and performance improvement programs for obstetrical services. The first deadline for these new requirements is July 1, 2025, so this year’s rulemaking is an important opportunity for CMS to signal whether it will stand by or revisit these policies. CMS could also use its CoP authority to address other administration priorities, such as its policies around diversity, equity, and inclusion (DEI), as expressed in the “Ending Radical and Wasteful Government DEI Programs and Preferencing” EO.
Each program is required by various statutes, but CMS has the authority to revise some of the measures included in each program. Historically, CMS has used that authority to add, refine, and eliminate measures through the IPPS. For example, in last year’s IPPS reg, CMS made changes to measures in the Hospital IQR Program, Hospital VBP Program, and PCHQR Program. CMS could make further changes to measures in these programs and other quality programs in parallel efforts to reduce administrative burden for hospitals, streamline the menu of available measures, and eliminate measures that may run counter to one of President Trump’s EOs, including his above-mentioned DEI EO.
Just as we did when we filled out our NCAA tournament brackets, we have provided our best predictions here about the timing and substance of the FY 2026 IPPS proposed reg. However, there could be some major upsets (such as surprise proposals), and we will have to wait to see what happens as the madness of reg season begins!
For more information, please contact Jeffrey Davis. To subscribe to Regs & Eggs, please CLICK HERE.
Until next week, this is Jeffrey (and Leigh) saying, enjoy reading regs with your eggs.